ADVERTISEMENTS:
Here is a term paper on the ‘Human Reproduction’. Find paragraphs, long and short term papers on the ‘Human Reproduction’ especially written for school and college students.
Term Paper on the Human Reproduction
Humans show sexual dimorphism. Males produce sperms and females produce ova. Fertilisation and development are internal. The primary sex organs are testes (male) and ovary (female). The growth of primary sex organs is controlled by gonadotropins secreted by anterior pituitary gland. Testes and ovary, other than producing the gametes also secrete hormones.
a. Gametogenesis:
ADVERTISEMENTS:
It is the formation of haploid gametes – sperm and ovum from diploid primary germ cells – gametogonia, i.e. spermatogonia in male and oogonia in female. In males the gametes are produced by the process of spermatogenesis and ova are produced in ovary by the process of oogenesis. The gametes originate from primordial germ cells (PGC). PGC originates from extra embryonic mesoderm during embryonic development.
There are two types of gametogenesis:
i. Spermatogenesis:
Generation of spermatozoa (haploid) from spermatogonia (diploid) is called spermatogenesis.
In some seasonally breading animals, the testes undergo testicular cycle. In this the spermatogenic tissue becomes active only during breeding season. In some cases testes remain in the abdomen for most of the period and descend in the scrotum only during the breeding season e.g. Llama, bat and otter. In some animals testes remain in the abdomen all through the life.
Testes are called intra-abdominal if they remain inside the abdomen. Spermatogenesis is a continuous process and it takes around 74 days for the process to complete itself. (Fig. 6 and 7)
Spermatogenesis takes place in two parts:
A. Formation of spermatid
This is further divided into three phases:
a. Multiplicative phase,
b. growth phase,
c. maturation phase and
B. Spermiogenesis.
ADVERTISEMENTS:
A. Formation of Spermatid:
a. Multiplicative Phase:
Seminiferous tubues of the testes contain germinal epithelium which harbours primordial germ cells or primary germ cells (diploid). These cells start dividing rapidly by mitosis. The cells so formed are undifferentiated and have chromatin rich, large nucleus. These cells become round and are now called as sperm mother cells or spermatogonia.
These spermatogonia are of two types – type A spermatogonia and type B spermatogonia Type. A cells act as stem cells and continue dividing by mitotic cell division. Type B cells move towards the centre and enter growth phase.
ADVERTISEMENTS:
b. Growth Phase:
In this phase diploid spermatogonia doubles in size by accumulation of nutritive material which is not synthesised but derived from germinal cells. Replication of DNA takes place and spermatogonia changes into diploid primary spermatocyte. This process is called as spermatocytogenesis. Now primary spermatocyte prepares itself to enter meiosis.
c. Maturation Phase:
During this phase diploid primary spermatocyte undergoes meiosis I (reductional division) and forms two haploid cells called secondary spermatocyte. This is followed by meiosis II. By the end of this process one haploid primary spermatocyte gives rise to four haploid secondary spermatocyte which after second meiotic division are known as spermatid.
ADVERTISEMENTS:
B. Spermiogenesis:
Transformation of non-motile spermatid into motile spermatozoon is known as spermiogenesis or spermioteliosis. During transformation of spermatid into spermatozoon following events occur.
RNA, protein and nucleolus is lost because of which nucleus is pushed anteriorly and becomes pointed, condensed and narrow. Some part of Golgi body is lost and is called Golgi rest and the remaining part forms the acrosome. Centriole forms neck and distal centriole forms the axoneme.
Mitochondria forms the spiral ring behind the neck around the distal centriole and proximal part of axoneme. This is known as nebenkern Small part of cytoplasm forms sheath of tail of sperm (Fig. 7).
Mature sperms are released in the lumen of seminiferous tubules. In young adult male around 120 million sperms are generated each day.
Role of Sertoli Cells:
Between the basal lamina and sertoli cells lie the spermatogonia.
Functions performed by Sertoli cells are as follows:
a. Sertoli cells provide nourishment to the developing spermatozoa. Because of this they are also known as nurse cells. Exchange of nutrients, gases and waste between developing spermatozoa and blood vessels takes place via the sertoli cells.
b. These cells provide mechanical support and protection to developing spermatozoa.
ADVERTISEMENTS:
c. Residual cytoplasm which is discarded during spermiogenesis is phagocytically consumed by sertoli cells.
d. Sertoli cells secrete fluid which helps in transportation of spermatozoa.
Spermatogenic function of testes is controlled by follicle stimulating hormone and androgen.
On the basis of sex chromosomes there are two types of sperms – sperms with X chromosomes called as Gymnosperm and sperms with Y chromosome called as Androsperm.
Sex Determination:
If the ovum is fertilised by a gymnosperm a female child is born and if the ovum is fertilised by an androsperm a male child is born.
ADVERTISEMENTS:
Hormonal Control of Male Sexual Functions:
Hypothalamus secrete Gonadotropin Releasing Hormone which stimulates the anterior pituitary gland to secrete Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) Luteinizing hormone stimulates the testes to secrete testosterone and follicle stimulating hormone stimulates spermatogenesis.
Testosterone is secreted by Leydig cells or interstitial cells of the testes. The amount of luteinizing hormone decides the amount of LH to be secreted. Sertoli cells secrete Androgen Binding Protein (ABP). The production of ABP is controlled by testosterone and FSH. ABP helps in concentrating testosterone in seminiferous tubules and stimulates spermatogenesis.
The secretion of FSH diminishes with increase in the process of spermatogenesis. This feedback effect on anterior pituitary is caused because of secretion of inhibit by Sertoli cells. With the secretion of excess of testosterone, there is automatic negative feedback effect, operating through the hypothalamus and anterior pituitary gland reducing the testosterone secretion back to normal (Fig. 8).
ii. Oogenesis:
Formation of haploid ova from diploid egg mother cells. Oogonia in females is called oogenesis.
Like spermatogenesis, oogenesis also has three phases:
a. Multiplication phase,
b. Growth phase and
c. Maturation phase (Fig. 9).
a. Multiplication Phase:
During this phase some primary germ cells which are larger in size and have a prominent nucleus of germinal epithelium undergo rapid mitotic division. This results in the formation of diploid egg mother cells called as oogonia. During initial stages each group resembles like a chord and so is called as egg tube of pfluger. This later forms a round mass called as egg nest.
b. Growth Phase:
During this phase one oogonium of egg nest changes into diploid primary oocyte. The rest of the oogonia form the nutritive follicular epithelium around the primary oocyte. This structure is called as primary oocyte Growth phase is a very long phase. In different animals it has different duration. In Drosophila it is for three days, in hen it is for 6-14 days and in humans it is as long as 12-13 years.
Following are the steps involved in growth phase:
i. Nucleus enlarges and is called germinal vesicle.
ii. Size of oocyte increases by about 200 times in humans. This is because of formation of yolk vitellogenesis.
iii. Vitelline membrane is secreted around oocyte.
c. Maturation Phase:
This is the phase when meiosis takes place. Meiosis I is a reduction division but the daughter cells so formed are of unequal size. The smaller cell is called as first polar body. This contains a very small amount of cytoplasm. The other daughter cell has larger part of cytoplasm and is called secondary oocyte.
This secondary oocyte undergoes meiosis II which is equational division. This division also gives rise to two unequal cells. The smaller daughter cell is known as second polar body and carries a very small portion of cytoplasm. The larger daughter cell, which has most of the cytoplasm, is called ootid.
This ootid differentiates into ovum. While this process is going on, first polar body may divide into two. This shows that during oogenesis one diploid oogonium forms one haploid ovum and two or three polar bodies. The significance of formation of polar bodies is to retain most of the cytoplasm in one cell and maintain haploidy.
In human female, ovulation occurs at the secondary stage in which meiosis I is over and meiosis II is completed at the time of sperm penetration.
Structure of Gametes:
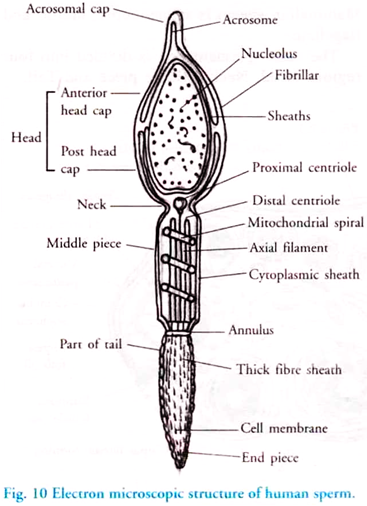
Structure of Human Spermatozoon (Fig. 10):
Mammalian sperm is microscopic, motile and flagellate.
The male spermatozoon is divided into four regions:
a. Head,
b. Neck,
c. Middle piece and
d. Tail.
a. Head:
Human sperm has got a flattened head. Head is made of two parts Acrosome and Nucleus. Acrosome is present at the tip of the nucleus and it is small and pointed. It mainly consists of golgi bodies and at the time of penetration into egg it secretes enzyme hyaluronidase which helps the nucleus to penetrate. Nucleus mainly consists of condensed chromatin material. This carries the genetic information. Both acrosome and anterior half of nucleus is covered with fibrillar sheath called galea.
b. Neck:
It is the smallest part of spermatozoon. It consists of two centrioles – proximal and distal centrioles placed perpendicular to each other. Both the centrioles are microtubular triple structure having 9 + 0 arrangement. Centrioles are responsible for the formation of spindle fibers during first zygotic cleavage. Distal centriole acts as basal body and gives rise to axoneme of tail.
c. Middle Piece:
It lies between the neck and tail. It is made of nebenkern, mitochondrial spiral. Since mitochondria carries enzymes- responsible for oxidative phosphorylation the middle piece is also known as power house of sperm. Posterior part of nucleus, neck and middle piece is covered by a sheath – manchette.
d. Tail:
This is the longest part of sperm which is flagellate. Tail is divided into outer and central part. Outer part is protoplasmic sheath whereas central part is called axoneme or axial filament. Axoneme is microtubular and has 9 + 2 arrangement of proteinaciuos tubules. Junction of middle piece and tail may have ring centriole. Tail helps in forward movement of sperm. Viability of human sperm is 24 hours.
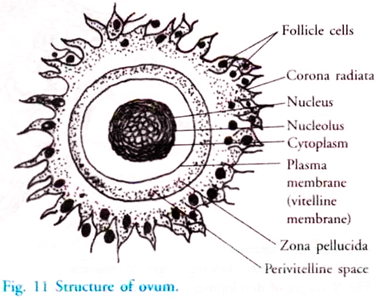
Structure of Ovum (Fig. 11):
Ovum is haploid female gamete which receives the sperm and develops into zygote. If fertilisation occurs it is called syngamy. If the development is without fertilisation it is named as parthenogenesis.
Human ovum is non-motile, round, much larger than sperm and alecithal, i.e. without yolk. Cytoplasm of ovum is called as ooplasm and nucleus is known as germinal vesicle. This is surrounded by plasma membrane known as vitelline membrane. During growth this vitelline membrane has microvilli which helps in absorbing nutrients from follicular cells.
The side of ovum which releases polar bodies is called as animal pole and the opposite side of this is known as vegetal pole. Next to the vitelline membrane is zona pellucida which is non-cellular, transparent, thin and made up of glycoprotein.
The outermost layer is the corona radiata which is thick and made up of elongated follicular cells. Space between zona pellucida and vitelline membrane is called as perivitelline space.
Menopause (Climacteric Period):
This is a period when ovulation and menstrual cycle stops. This takes place between the ages of 45-55 years. Menopause is characterised by hot flushes and a number of psychic symptoms. During this phase FSH is secreted in urine. Menopause occurs because of decline of estrogen.
In case of male the function of testes declines slowly because of decrease in level of testosterone. This is known as male climacteric.
Menstrual or Ovarian Cycle (Fig. 12):
In human female the reproductive phase is for 30-33 years. This starts at the puberty age and ends with menopause. During this phase the reproductive tract and the ovary undergoes cyclic changes which are meant for fertilisation and the preparation of reproductive tract to receive fertilised egg.
This cyclic process is called menstrual cycle. Most prominent activity of this phase is the vaginal bleeding which is known as menstruation. This menstrual cycle, on an average is completed in 28 days though, it may vary from individual to individual.
Menstrual cycle is absent during pregnancy, may not occur during lactation and completely stops on commencement of menopause.
Menstrual cycle is divided into four phases, Follicular/Proliferative/Post-Menstrual/Pre-ovulatory phase, Ovulatory phase, Luteal/Progestational/Pre-menstrual/Secretory/Post-ovulatory phase and menstrual phase.
a. Follicular/Proliferative/Post-Menstrual/Pre-Ovulatory Phase:
It lasts for 10-12 days and is followed after menstrual phase.
Following changes occur during this phase:
i. Under the influence of FSH-RF of hypothalamus, secretion of FSH increases from the anterior pituitary.
ii. FSH enhances the change of primary follicle of ovary into Graafian follicle.
iii. Estrogen is secreted by the follicular cells of Graafian follicle.
Estrogen stimulates the maintenance, growth and normal functioning of secondary sex organs. It also makes uterine endometrium thick, vascular and more glandular. Estrogen inhibits the secretion of FSH and stimulates the secretion of LH. Glycogen and fat accumulation in endometrial cells is also regulated by estrogen.
b. Ovulatory Phase:
This is the 15th day of menstrual cycle and involves the ovulation from Graafian follicle. It is caused by contraction of smooth muscle fiber and turgidity around the Graafian follicle. Fimbriae of fallopian tube receives the ovum. Life span of ovum is 48 hours. Increased level of LH controls ovulation. LH also helps in changing the empty Graafian follicle into corpus luteum and in secretion of progesterone from corpus luteum.
c. Luteal/Progestational/Pre-Menstrual/Secretory/Post-Ovulatory Phase:
It starts from the 16th day of menstrual cycle and lasts for 12-14 days.
Following are the changes, which occur during this phase:
i. Corpus luteum increases in size.
ii. Progesterone is secreted by corpus luteum and its level increases in the blood. This decreases the secretion of FSH and LH which inhibit the maturation of follicle and ovulation. Due to high level of progesterone uterine endometrium proliferates further and it also reduces the uterine movement.
d. Menstrual Phase:
It extends from 1st to 4th day of menstrual cycle and lasts for 3-4 days. If the ovum is unfertilised then the corpus luteum starts degenerating. The level of progesterone declines in the blood. Due to this the uterine tissues cannot be maintained. So, unfertilised ovum with ruptured uterine epithelium, some mucous and 50-100 ml of blood is discharged through the vaginal orifice and is called menstrual flow or menstruation.
As the level of estrogen and progesterone decreases in the blood, it stimulates the hypothalamus and anterior pituitary to release FSH – RF and FSH respectively. FSH starts the follicular phase of next menstrual cycle. This is called positive feedback.
In case of fertilisation, zygote changes to blastula and gets implanted and a chorionic placenta is formed. Human Chorionic Gonadotropin (HCG) maintains the corpus luteum and the secretion of progesterone continues. Progesterone helps in the maintenance of pregnancy and prevents ovulation till the gestation period continues.
Hormonal Control of Female Sexual Function (Fig. 13):
The process of oogenesis is controlled by three endocrine glands – hypothalamus, anterior pituitary gland and ovaries.
The hormones released are Gonadotropin Release Hormone from hypothalamus, Follicle Stimulating hormone and Luteinizing hormone secreted by anterior pituitary and Estrogen and Progesterone from the ovaries.
Hormonal pattern can be understood by following the normal monthly cycle of development of ovum and the physical events in the menstrual cycle.
The sequence is as follows:
a. Controlling center of menstruation and ovulation is the hypothalamus. It releases GnRH, which stimulates the release of FSH and LH from the anterior pituitary.
b. FSH initiates the development of the oocyte within one of the immature ovarian follicles.
c. Ovarian follicle produces Estrogen, which causes the build-up of endometrium as well as the inhibition of further production of FSH.
d. The increased level of estrogen stimulates the anterior pituitary to secrete LH, which helps in enlarging the mature follicle and releases the secondary oocyte. It also helps in changing the collapsed follicle into corpus luteum, an endocrine body.
e. Estrogen and Progesterone are secreted by corpus luteum. This helps in completing the development of endometrium.
f. If the oocyte is not fertilised and not implanted in the endometrium, the corpus luteum disintegrates and is known as corpus albicans, and estrogen and progesterone secretion is stopped.
g. Without progesterone and estrogen, the endometrium breaks down and menstruation occurs.
h. The level of progesterone decreases further, and the level of LH drops off too. This decrease in LH causes pituitary to start secretion of FSH, which stimulates the development of another ovum. The cycle begins again.
Embryonic Development:
Embryonic development includes the transformation of single cell zygote into a multicellular and fully developed young one.
This takes place through a series of phases, which is quite similar in all the sexually reproducing animals. On studying the embryos of different animals striking similarity is seen between them, proving that all metazoans are interrelated and have common ancestry.
Phases of Embryonic Development:
Embryonic development can be divided into five phases:
a. Gametogenesis:
Formation of gametes by the process of spermatogenesis and oogenesis.
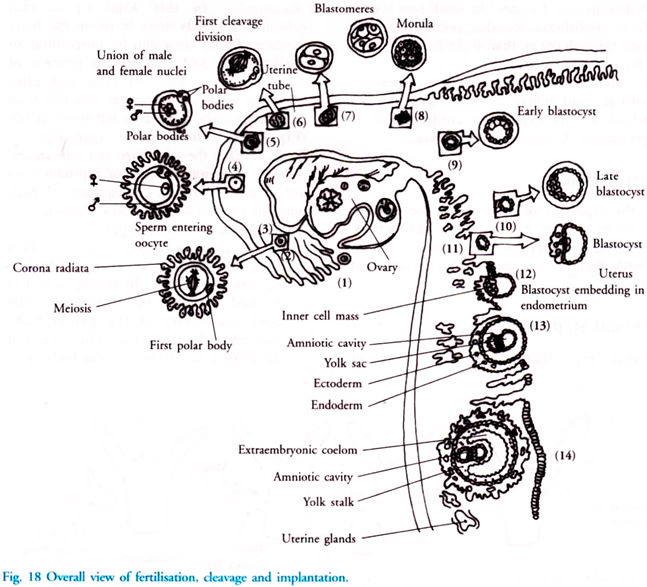
b. Fertilisation:
Union of male and female gametes (Fig. 14).
c. Cleavage and Blastulation:
Successive and rapid mitotic divisions in the zygote, changing it into ball or disc like structure. Cells forming this structure are called blastomere. This results in the formation of blastula. The blastomeres enclose a space called as blastocoel.
d. Gastrulation:
In this the blastomeres move from the surface by the process of invagination and reach the pre-determined position and form three germinal layers.
e. Organogenesis:
During this phase the three germinal layers give rise to specific tissue, organ and organ system. It includes differentiation of cells and tissues and morphogenesis.
Arrival of Sperm:
Semen is discharged high up in the vagina close to the cervix. This is called insemination. Each ejaculation contains 3.5 ml of semen and around 400 million sperms. These sperms swim in the uterus at a speed of 1.5 to 3 mm per minute. It takes a few hours for the sperm to reach the uterine tube (15-20 cm).
Most of the sperms are killed because of the acidity in the female genital tract. Many sperms are taken by the vaginal epithelium by the process of phagocytosis. Due to this only 100 sperms are able to reach the oviduct. This is the reason of having such a large number of sperms in the beginning.
Hormone oxytocin which is released during copulation and prostagland in which is present in the semen help in the movement of sperms by causing peristaltic movement in fallopian tube and aspiratory action of uterus.
Arrival of Ovum:
The egg which is released from the ovary is received by the fallopian funnel and moves towards the oviduct by the ciliary movement of cells of fallopian duct. Ovum is in the secondary oocyte stage. Only one sperm fertilises the egg whereas the others degenerate.
Penetration of Sperm:
At the animal pole, sperm comes in contact with ovum. Penetration is a chemical process during which acrosome releases certain lysins which help in dissolving the egg envelop. Sperm lysins are proteins and acidic in nature.
Lysins have enzyme hyaluronidase which dissolves hyaluronic acid polymer in the intercellular spaces of cells of corona radiata. It also dissolves the zona pellucida. The penetration is only of the nucleus and the middle piece.
With the penetration of sperm, cortical granules appear in the egg cortex. Perivitelline space is created. Some of the cortical granules move in this perivitelline space and attach to the inner surface of the vitelline membrane. This membrane thickens and now is called as fertilisation membrane It prevents polyspermy.
Entry of sperm stimulates the completion of meiosis, which produces the ovum and second polar body. The chromosome of sperm and ovum mix and this is known as amphimixis. The fertilised egg is now known as zygote Nucleus of zygote is known as synkaryon.
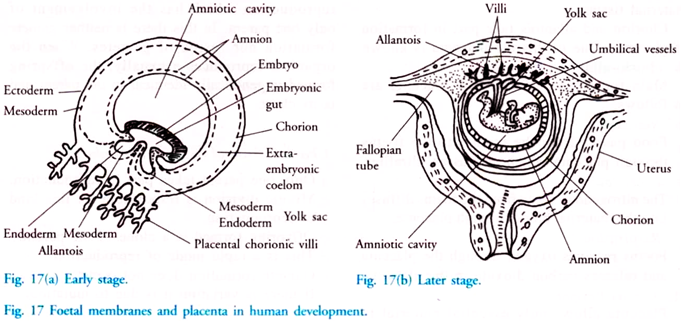
a. Cleavage:
Successive and rapid mitotic divisions in the zygote, changing it into ball or disc like structure. Cells forming this structure are called blastomere. This results in the formation of blastula. The blastomeres enclose a space called as blastocoel. This process is known as blastulation.
During cleavage there is no growth of cells, so the cell size becomes smaller and smaller. This type of cleavage is called fractionating process Due to increase in DNA and no addition of cytoplasm the nuclear- cytoplasmic ratio keeps on increasing. Initially the blastomeres show synchronous division but, it is lost after some time.
Cleavage starts in the fallopian tube, as the zygote moves towards the uterus. After a few cleavages the zygote resembles a little mulberry so it is called morula. Morula is the 32 cell stage and it takes four days to reach the uterus.
Next step is formation of blastula. This involves rearrangement of blastomeres. Outer cells are flat and are called trophoblast. The fluid which is absorbed by these cells is collected in a central cavity called blastocoel. With increase of fluid in blastocoel, the size of morula increases and now it is known as blastocyst.
b. Gastrulation:
In this process the blastomeres move from the surface by the process of invagination and reach the predetermined position and form three germinal layers.
The movement of blastomeres is interdependent and is called morphogenetic movement As a result of this movement the blastula changes to gastrula and the formation of three germinal layers, i.e. ectoderm, mesoderm and endoderm takes place. Each germ layer gives rise to specific tissues, organ and organ system.
c. Organogenesis:
During this phase the three germinal layers give rise to specific tissue, organ and organ system. It includes differentiation of cells and tissues and morphogenesis.
Ectoderm gives rise to:
i. Chromatophores, i.e. pigment cells of skin
ii. Nervous system
iii. Epidermis of skin, epidermal glands, hair, nails
iv. Conjunctiva, ciliary muscle, cornea and lens of eye
v. Nasal and olfactory epithelium
vi. Outer layer of tympanic membrane and internal ear
vii. Enamel of teeth
viii. Sweat gland, mammary gland, sebaceous gland, lacrimal gland, pituitary gland, salivary gland, medulla of adrenal gland and pineal gland
ix. Epithelial lining of foregut and hindgut.
Mesoderm gives rise to:
i. Connective tissue
ii. Dentine of teeth
iii. Dermis of skin
iv. Blood and lymph
v. Spleen
vi. Notochord
vii. Heart and blood vessels
viii. Cortex of adrenal gland
ix. Coelomic epithelia
x. Most of the skeleton
xi. Mesenteries
xii. Excretory system except urinary bladder and urethra
xiii. Reproductive system except the prostate
xiv. Sclera and choroid of eye.
Endoderm gives rise to:
i. Urinary bladder and urethra
ii. Inner layer of tympanic membrane
iii. Trachea, bronchi and lungs
iv. Epithelial lining of Eustachian tube and tympanic cavity
v. Mucous membrane of the gut except foregut and hindgut
vi. Pancreas, gastric gland, liver, intestinal gland, thyroid, parathyroid, thymus.
Human Extra-Embryonic Membrane or Foetal Membrane in Human Development:
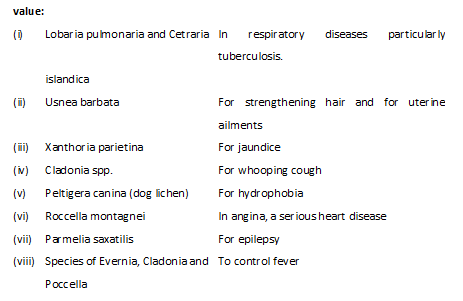
These membranes are formed as the implantation starts. There are four membranes amnion, chorion, allantois and yolk-sac. (Fig. 17)
a. Amnion:
On the inner side it is made of ectoderm and outer side is mesoderm. Amniotic cavity is formed between the embryo and amnion. It is filled with amniotic fluid. This fluid is clear and watery and is secreted by both membrane and embryo. It helps in absorbing shocks and acts as a protective cover for the growing foetus.
b. Chorion:
On the outer side it is made of ectoderm and inner side is mesoderm. It surrounds the embryo and helps in the formation of placenta. It also protects the embryo.
c. Allantois:
It arises near the yolk sac and is sac like. Towards inside it is made of endoderm and outside it is mesoderm. It is non-functional in human beings except that it forms the urinary bladder and a few blood vessels to the placenta.
d. Yolk-Sac:
Yolk-sac is made of endoderm towards inside and mesoderm outside. In human’s part of it forms the site of blood cells formation and part gives rise to germ cells.
Placenta in Human Development:
It is a temporary, physiological, mechanical and intimate connection between foetal and maternal tissues.
Chorion and allantois take part in formation of placenta. Due to this the placenta is known as chorio-allantoic placenta.
ADVERTISEMENTS:
Main functions performed by placenta are as follows:
a. Nutrition:
Food passes from the mother to the foetus through placenta which acts as an ultra-filter.
b. Excretion:
The nitrogenous waste from the foetus diffuses into the maternal blood through placenta.
c. Respiration:
Foetus receives oxygen through the placenta and releases carbon dioxide in the placenta.
d. Acts as Barrier:
Placenta allows only essential material to pass towards the foetus.
e. Transport of Antibiotics:
Antibiotics for diseases like small pox, scarlet fever, diphtheria, measles, tetanus, etc. can pass through the mother to the foetus.
f. Functions as Endocrine Gland:
It secretes hormones as progesterone, estrogen and human chorionic gonadotropin which are necessary for continuation of pregnancy. It also releases relaxin.
Parturition:
It is the expulsion of fully grown foetus from the uterus at the end of gestation period. Gestation period is the time from conception till birth. Parturition is controlled by relaxin and oxytocin.