ADVERTISEMENTS:
Let us make an in-depth study of the nanomedicines. The below given article will help you to learn about the following things:- 1. Introduction to Nanomedicines 2. Barriers to Nanoparticles Distribution 3. Extravasation of Nanoparticles 4. Passage of Nano-Materials through Tissues 5. Uptake into Cells 6. Biodistribution & Nanoparticle Penetration and 7. Implications for Nanotoxicology from Nanomedicines.
Introduction to Nanomedicines:
Nanotechnology has a very broad definition based on scale, and Nano medicines are likewise based not only on the type of medicine or their function but also on a Nano sized range. While most nanotechnology is expected to have an upper size limit of 100 nm, in the drug delivery field this is more generally accepted as medicines in the size range from a few nanometers to 1,000 nm in diameter.
In practice, the useful range of Nano medicines more normally falls within the range of 5-250 nm as these tend to have a similar range of properties based on physiological and anatomical consequences. In the next few paragraphs we examine some basic pharmaceutical principles and some anatomy to see why this is the case.
ADVERTISEMENTS:
Traditionally, chemists have produced drugs by exploring small molecules and their structures to produce pharmacologically active materials. These small molecules are typically in the molecular weight range of 100-500, although some larger molecules are in general use.
Also typically, these molecules are designed to have a useful combination of lipophilicity and hydrophobicity so that they have some solubility in an aqueous environment, but are sufficiently hydrophobic to partition through membranes. These properties mean that they distribute all over the body fairly rapidly via the circulation and by diffusion through tissues and cells.
Their hydrophobicity enables them to be sufficiently soluble to interact with their target, which is usually found in an aqueous environment. Specificity is achieved by interaction with their target, typically a pharmacological receptor or an enzyme. The action and distribution of these traditional medicines are therefore mainly governed by their chemical structure and their physiochemical properties. For the last three or more decades the term ‘Nano medicine’ can cover a wide variety of materials and structures (see Fig. 13.1).
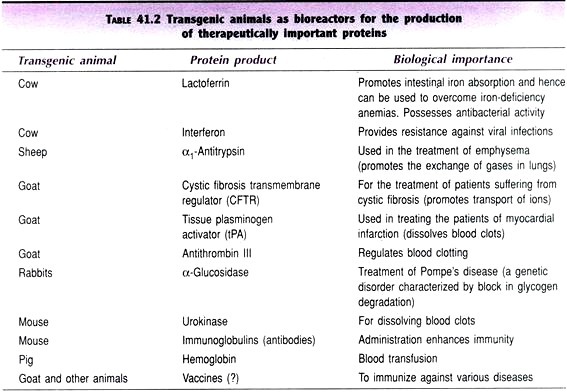
In general, they have been around for considerably longer than they have been known as Nano medicines, and some have been investigated. The sort of materials that could be called Nano medicines can include proteins, polymers, dendrites, micelles, liposomes, emulsions, nanoparticles and Nano capsules.
ADVERTISEMENTS:
Nano-materials are also used in diagnostics, e.g. colloids for radio pharmacy and as contrast agents in magnetic resonance imaging. New development in Nano-materials are now producing small and ultra-small paramagnetic iron oxide particles (USPIOs) and investigating quantum dots for this field. In general, Nano-materials of this size are not able to penetrate membranes readily, and consequently are mostly dependent on the anatomy and physiology of the body to determine their distribution:
Barriers to Nanoparticles Distribution:
In general, biological compartments act as barriers to the passage of Nano sized materials, and there are several barriers to consider. Firstly, the epithelium acts as a general barrier to prevent ingress of materials into the body.
However, in this article we only consider the fate of particles which have got past this barrier, e.g. by parenteral injection, and how they travel and distribute within the body. Looking first at the blood and circulation, the body has a number of defenses against particulate materials, as naturally these are living organisms such as bacteria, viruses and protozoa.
Such particulate materials tend to be hydro- phobic and are readily coated by serum proteins which act as opsonins. These opsonins, principally antibodies and complement factors, facilitate the binding of nanoparticles to phagocytic cells, particularly macrophages and neutrophils which take them up.
There are high concentrations of phagocytic cells in the organs of the mononuclear phagocytic system, principally liver, spleen and lymph nodes, and typically the majority of opsonized particles are cleared from the circulation to the liver and spleen in 5 min.
However, coating these particles with flexible hydrophilic polymers, particularly polymers containing polyethylene glycol (PEG), can reduce opsonization of the particles and allow them to remain in the circulation for much longer periods. Once circulating for longer periods, these particles can be carried round the body and reach other tissues and cells, other barriers permitting.
Extravasation of Nanoparticles:
The next barrier to nanoparticle distribution is the vascular endothelium. Typically most endothelium is continuous with tight junctions between the endothelial cells and the underlying basement membrane. The presence of tight junctions means that the gap between endothelial cells is 2 nm, thus preventing most nanoparticles from exiting the circulation by passage between the cells (Para cellular route). Even if materials are able to pass through the endothelial cells, the network of the underlying basement membrane would be expected to limit passage of materials larger than 13-15 nm in diameter.
In some specialized tissue like liver, the endothelium is fenestrated, thus allowing material up to 100 nm to pass from the endothelium to the underlying parenchymal cells. In other tissues like spleen, the endothelium is discontinuous, having larger fenestrations, and also lacks basement membrane, allowing exit of very large particles.
ADVERTISEMENTS:
In contrast, in the brain the endothelial junctions are particularly tight and effective, reducing still further the ability of materials to pass through (the blood-brain-barrier). In addition to the Para cellular route of exit from the circulation, some materials can also pass through the endothelial cells in a process known as transcytosis, a process involving caveolae. This allows the passage of macromolecules through the endothelium, and is thought to be size- dependent, so larger macromolecules pass through less easily than smaller molecules.
Also, under certain disease conditions, e.g. inflammation, the endothelium can become leaky, allowing a greater exit of particulate materials. In some cancers the endothelium not only becomes leaky but also loses the lymphatic’s, leading to accumulation of materials in tissues, a process termed the enhanced permeability and retention (EPR) effect (see Fig. 13.2).
By exploiting processes like the EPR effect, nanotechnology could thus be useful in improving delivery of drugs to particular sites in the body and thus helping to control the effectiveness and side effects of drugs by controlling the location the drugs can reach.
Passage of Nano-Materials through Tissues:
ADVERTISEMENTS:
Once out of the circulation, Nano-materials will be present in the extracellular matrix. Any spaces between the cells are filled with an aqueous gel composed mainly of proteins such as collagen, polysaccharides such as hyaluronic acid and glycoproteins such as chondroitin sulphate. These usually form a tangled matrix that impedes movement of molecules.
However, the nature of the matrix is that some water channels are present and these may permit the passage of some macromolecules and particles in the same way that is seen in a gel permeation chromatography column, where macromolecules move faster through the matrix than do small molecules.
Uptake into Cells:
As partitioning across membranes is not possible for macromolecules, entry into cells is largely governed by biological mechanisms of endocytosis. These include the uptake of large particles (0.25-10 mm) by phagocytosis, performed by specialized cells such as macrophages and neutrophils, and a variety of other endocytic processes at a smaller scale.
The routes of endocytosis most prominently described in the literature in recent years are the receptor-mediated routes. These routes require recognition of some ligand (surface molecule or epitope) by a specific biological receptor.
ADVERTISEMENTS:
The best known of these, clathrin-mediated endocytosis, involves a vesicle of a defined size of 100 nm, and can promote uptake through a number of different routes through the cell. A second mechanism, more recently described, is potocytosis involving caveolae, flask-shaped vesicles of 70 nm diameters.
The routes, specific ligands and mechanism of uptake of this second route are less clear. However, the receptor-mediated routes of uptake do not account for all uptakes of material into cells, and other mechanisms—which could come under the term pinocytosis described in earlier literature and which can account for modes of uptake not involving receptors—must also be operative.
These routes of uptake, which include macro-pinocytosis, can potentially allow uptake of materials up to 300 nm in diameter. All these endocytic routes of uptake involve delivery of material into a subcellular compartment, the endosome, which is still separated from the cytoplasm of the cell by a membrane. Most of these endocytic routes also end up in a degradative compartment of the cell, the lysosome, where materials are exposed to high concentrations of a wide variety of hydrolytic enzymes active on proteins, polysaccharides and nucleic acids.
More recently, some uptake of particles directly into the cytoplasm of cells has been reported in the literature. Uptake of small hydrophobic particles by macrophages has been described and celled patocytosis. This process has been characterized as size dependent, not occurring for particles larger than 500 nm and associated with the process of capping, in which the particles become trapped in membrane folds which remain open to the intracellular space.
ADVERTISEMENTS:
However, a further report described the uptake of small hydrophobic particles into macrophages and a range of other cell types including red blood corpuscles. The major difference in this second report was that particles were not membrane bound, but in direct access with intracellular proteins and organelles.
A second type of mechanism where particles may have direct access to the cytoplasm is with strongly positively charged particles. It is well-known that positively charged polymers and polyelectrolyte DNA delivery systems can because toxicity mediated through membrane effects.
Recent work with dendrimers has shown that positively charged dendrimers can cause membrane defects 15-40 nm in diameter which leak cellular proteins and through which particles can pass. It is not yet clear how widespread these non-vesicular particle uptake mechanisms are, or what range of surface characteristics can mediate these membrane- crossing events.
Biodistribution and Nanoparticle Penetration:
From the above description of the physiology and anatomy, we would expect the bio distribution of nanoparticles to be very limited, uncoated particles being rapidly taken up by the spleen and liver, mainly by macrophages. If suitable coatings can be applied to nanoparticles, it would be expected that they would largely remain in the vasculature, until gradually eliminated by similar scavenger mechanisms, as it should be difficult for these materials to pass across the endothelium. However, a number of results now suggest that nanoparticles may accumulate in other tissues.
The first indication of specific sites of accumulation for nanoparticles was seen in early work on the bio distribution of model polystyrene nanoparticles coated with poloxamers. These detergents adhere to particle surfaces through their hydrophobic regions, and the hydrophilic segments protrude into the aqueous medium.
Particulate formulations of these particles were found to accumulate to significant extent in the bone marrow and were in fact shown to be located in the sinusoidal bone marrow endothelium. Later work, using polybutyl cyanoacrylate particles coated with the surfactant Tween 80, showed other sites of accumulation.
ADVERTISEMENTS:
Small but significant amounts of particles were found to accumulate in brain tissue. This accumulation was in the brain cells beyond the blood-brain-barrier, and again it was shown that transfer across the endothelium had occurred. In this case the transfer was shown to be mediated by a specific uptake mechanism involving Apo-lipoprotein E, which was selectively adsorbed to the nanoparticle surfaces. Other formulations of these particles were also shown to accumulate in the gut.
More recently, another example of accumulation in a specific tissue has been seen. Nanoparticles of iron oxide coated with starch have reportedly been found in the lymph nodes, again after passage through the endothelium. Very small iron oxide formulations (USPIO) can be stabilized with dextran, and remain in the circulation for some time. However, this recent observation caused some surprise, as these particles were quite large (90 nm) and not very efficient at remaining in the circulation, yet still managed to localize in a particular compartment.
Taken together these observations suggest that endothelium varies within different tissues, and that even nanoparticles with simple coatings can accumulate selectively in certain specific areas of the body, although usually only as a small proportion of the administered dose. Once outside the circulation, the evidence on how well materials can cross certain tissues is more limited. One area of evidence comes from studies of nanoparticles injected intradermal or subcutaneously.
These are essentially materials that have been injected into the extracellular matrix, their potential route away from the injection site being by drainage through the lymphatic vessels, through the lymph nodes and back to the circulation. This route was explored for its potential to target materials to the lymph nodes. Uncoated nanoparticles tend to remain at the injection site. However, if the particles have
ADVERTISEMENTS:
PEG coatings, a proportion can drain from the injection site. The thickness of the coating is important; if a thin coating is applied, the materials get as far as the lymph nodes where they accumulate, but if a thicker coating is applied, they can escape the lymph nodes and get back to the circulation, but are then usually captured by the liver macrophages. However, this does illustrate that channels exist within the extracellular matrix for these particles to move along. In these studies a particle size of only 60 nm was important.
ADVERTISEMENTS:
Some further evidence exists for similar channels in the brain. When ferritin was injected into the cerebrospinal fluid of rats, these macromolecules did pass into the brain tissue, and many of these particles were seen passing quite deeply into brain tissue through a number of small channels. Ferritin has an iron core of ~9 nm with a protein outer coat, so these particles are somewhat smaller, but still demonstrate the principle that larger particulate materials can pass intact through tissues. The general principle for the uptake of nanoparticles into cells through endocytic routes is now well-accepted.
Discussion in many review articles suggest that for this process to occur efficiently particle sizes need to be 100 nm, because they will be limited by the size of vesicles, on the assumption that all endocytic vesicles will be smaller than 100 nm. However, this assumption does not seem to be borne out in practice. In the field of non-viral gene therapy, particles of various sizes have been generated to encapsulate DNA and uptake into cells is a prerequisite for obtaining protein expression through the process of transfection.
In this field there have been mixed results as to which formulations are most effective, but there are certainly many reports that large particle sizes, in the hundreds of nanometers range, are effective at protein expression.
Similarly, scientists have carried out cell culture work on using nanoparticles as drug carriers which have been produced from a new polymer, polyglycerol adipate (PGA). PGA is modified with pendant side chains that allow an efficient incorporation of rhodamine dye, and produce nanoparticles in a narrow size range ~ 175 nm diameter.
These nanoparticles are taken up consistently and rapidly by a medulla oblongata cell line and a variety of normal non-macrophage brain cells grown in either monolayer or three-dimensional cultures.
These studies strongly suggest that uptake of nanoparticles is not restricted to sizes, 100 nm and that therefore the reference to macro-pinocytosis in the older scientific literature is well justified. The results are important in developing Nano medicines, as delivery to this intracellular compartment provides a means to release the drugs. However, it also has toxicological implications for uptake of nonmedical nanoparticles.
Implications for Nanotoxicology from Nanomedicines:
Nanoparticles could come from many sources. Those developed specifically as medicines have been under development for many years. As part of this development process, the materials and strategies developed for this work have been chosen to minimize the possibilities of causing adverse and toxic effects, in particular the choice of biodegradable, biocompatible materials and the development of surface coatings which avoid the accumulation of nanoparticles in the liver and spleen.
Non-medical nanoparticles, which may be found in atmospheric pollution or produced in industrial processes, are unlikely to have these advantages, and their toxicology will be largely determined by the materials they are composed of and their surface characteristics.
The latter will determine where they eventually accumulate. Many airborne nanoparticles are likely to have a hydrophobic surface and will, therefore, be prone to accumulation in the spleen and liver. However, a number of industrially produced Nano-materials do need to be treated to prevent aggregation, and such stabilized materials are likely to behave in a similar manner to the stabilized Nano medicines designed to circulate in the vasculature.
Whichever path is followed, whether involving stabilized or unsterilized particles, there are potentially toxic consequences predictable from physiology and anatomy. Non-degradable nanoparticles which accumulate intracellularly are likely to have number of effects.
If taken up by macrophages, they would undoubtedly stimulate free radical release which may result in cell damage and inflammation. If the nanoparticles are taken up into the lysosomal compartment but are not biodegradable, they could potentially accumulate there and cause toxicity. This is clear by analogy with the variety of lysosomal storage diseases known, where lack of a degradative enzyme inevitably results in accumulation of material and toxic effects.
With any nanoparticle preparation, whether coated or not, a large proportion of administered dose finds its way to the liver, and so this is the organ most likely to be affected. In terms of other tissues, the endothelium is another tissue in direct contact with the nanoparticles.
The endothelium is itself a mediator of a large number of physiological responses, so there are possibilities for toxicity here; however, its role in mediating uptake to particular tissues is now also seen to be of significance. Accumulation in spleen, gut, bone marrow, lymph nodes and brain is already known to be possible, but there are also possibilities not so far reported that other organs may also mediate uptake via the endothelium.
In some cases such as the brain, only small proportions of circulating materials accumulate, so adverse effects are unlikely unless the materials are extremely toxic. However, in other tissues such as bone marrow or gut, the amount of accumulation could be substantial with more materials having a possibility of toxic effects.