ADVERTISEMENTS:
In this article we will discuss about Mycobacteria which causes Tuberculosis in man:- 1. Classification of Mycobacteria 2. Laboratory Diagnosis 3. Biochemical Reactions 4. Identification 5. Treatment 6. Immuno-Prophylaxis (by BCG Vaccine) 7. Dose and Administration.
Contents:
- Classification of Mycobacteria
- Laboratory Diagnosis
- Biochemical Reactions
- Identification
- Treatment
- Immuno-Prophylaxis (by BCG Vaccine)
- Dose and Administration of BCG Vaccine
1. Classification of Mycobacteria :
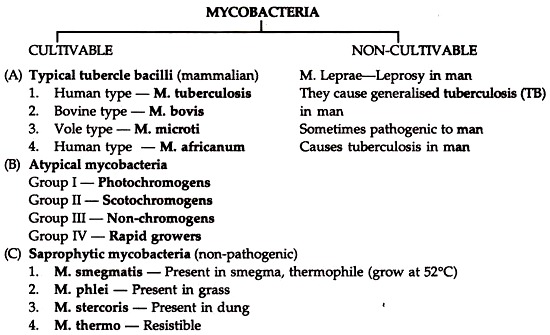
Mycobacterium tuberculosis (Human type) causes tuberculosis in man.
Morphology and Staining:
M. tuberculosis are thin straight acid fast bacilli (AFB) Stained by Ziehl Neelsen method; measuring 3 x 0.3 µm. In smears of sputum and sections of tissue, they can be demonstrated by yellow orange fluorescence after staining with fluorescence dye (e.g. auramine, rhodamine), non-motile, non-sporing, non-capsulated.
Cultural Characteristics:
ADVERTISEMENTS:
They are aerobes, grow slowly at 37°C. On Lowenstein-Jensen medium, their growth is more luxuriant (i.e. “eugonic“) than bovine type (dysgonic) they form thin, white, smooth, slightly moist, wrinkled, granular and easily broken up growth. Glycerol favours the growth of human type. Biochemical activities are not characteristic.
Pathogenicity:
The most common forms of primary infection is a pulmonary lesion which may be due to inhalation of organisms in very small particles into the alveoli, then it is carried by lymphatic drainage to the regional lymph nodes which are enlarged and followed by caseation and calcification.
Clinical features:
The clinical manifestations are different as the tubercle bacilli involve every organ system. Fatigue, weakness, weight loss and fever are main signs. Pulmonary involvement may give rise to chronic cough and splitting of blood in advanced cases. Meningitis or urinary tract infection may occur.
2. Laboratory Diagnosis of Mycobacteria:
A. Specimens:
Sputum, urine, pleural, spinal, joint, fluid, biopsy materials.
B. Smears:
Sputum and other specimens are examined for acid fast bacilli by Z-N method or by fluorescence microscopy with auramine rhodamine stain. If AFB are present, it is suggestive of mycobacterial infection.
ADVERTISEMENTS:
C. Concentration for stained smears:
If the dried smear is negative, sputum may be liquefied by addition of 20% chlorine bleach (1% hypochlorite solution) and then centrifuged. The sediment is stained and examined microscopically. The “digested material” should not be used for culture.
D. Culture:
Specimens are first treated with 2% sodium hydroxide, neutralized and centrifuged. The sediment is inoculated into the approximate medium and incubated up to 4-8 weeks. Isolated mycobacteria should be identified and tested for drug sensitivity.
ADVERTISEMENTS:
E. Serology:
DNA probes and Polymerase Chain Reaction (PCR) can detect even single Mycobacterium tuberculosis in clinical specimens with 100% sensitivity. ELISA is the method of choice compared to CFT agar gel diffusion. HA, Radio-immunoassay gives promising result. Active infection cannot be proved by tuberculin or serological test.
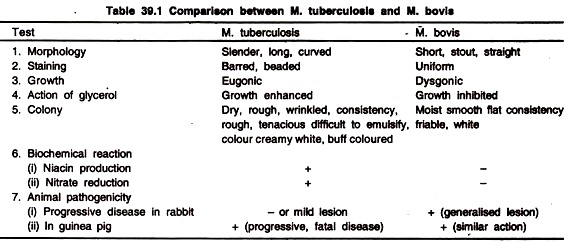
3. Biochemical Reactions of Mycobacteria:
Though the biochemical activities are not characteristic, they can distinguish different species of Mycobacteria:
1. Niacin Test:
ADVERTISEMENTS:
Only M. tuberculosis produces niacin, a nicotinic acid, in sufficient quantity during their growth in egg medium to give positive test. When a freshly prepared reagent (containing 10% cyanogen bromide and 40% aniline in ethanol) is added to a suspension of bacterial culture, a canary yellow colour develops showing positive reaction. Cultures of M. cheloneii and M. simiae also give positive niacin test.
2. Aryl Sulphatase Test:
The test becomes positive in culture of atypical mycobacteria as they produce the enzyme aryl suphatase. The atypical mycobacteria are first grown in media containing tripotassium phenolphthalein di-sulphate (0.001 M) for 2-4 weeks, when 0.2 N NaOH is added drop by drop, a pink colour develops in positive reaction due to the liberation of free phenolphthalein.
3. Catalase Test:
ADVERTISEMENTS:
Most atypical mycobacteria are strongly catalase positive and peroxidase negative. The tubercle bacilli (M. tuberculosis, M. bovis) are peroxidase positive and weakly catalase positive. They loose peroxidase and catalase activity when they become isoniazid (INH) resistant. Strains are avirluent to guinea pigs.
The reagent is prepared by mixing equal volume of 30% vol. H2O2 and 0.2% catechol in distilled water. This reagent is added to a 5 ml test culture in phosphate buffer (pH 7) at 68°C in a water bath and left for a few minutes for the reaction to occur. Catalase production is indicated by the effervescence and peroxidase activity by growing of colonies.
4. Identification of Pathogenic Mycobacteria:
If AFB are present
A. Growth in less than 7 days (rapid growers):
Positive aryl sulfatase test (3 days), growth on MacConkey’s agar
(a) Nitrate reduction positive—M. fortuitum
ADVERTISEMENTS:
(b) Nitrate reduction negative—M. cheloneii
2. Negative aryl sulphatase test—various non-pathogenic Mycobacteria.
B. Growth in more than 7 days (Slow growers) — if non-pigmented expose to light for 2 hours, then reincubate for 18 hours.
1. Non-pigmented growth:
ADVERTISEMENTS:
(a) Niacin test positive, nitrate reduction positive—M. tuberculosis.
(b) Niacin test negative, nitrate reduction variable—Mycobacteria other than M. avium intracellular.
2. Pigmented growth:
(a) Pigmented when grown in light, non-pigmented in dark—Photochromogen-M. kansasii.
(b) Pigmented when grow in light or dark—Scotochromogen—M. scrofulaceum. Acid fast bacilli—which are neither human or bovine type—cause human diseases, they are called anonymous or atypical mycobacteria.
“Atypical mycobacteria” were initially grouped as:
(a) Photochromogen M. kansasii.
(b) Scotochromogen—M. scrofulaceum
(c) Non-photo-chromogen—M. avium intracellular
(d) Rapid growers
5. Treatment of Pathogenic Mycobacteria:
In addition to physical, mental rest, nutritional build up, the specific chemotherapy (isoniazid, rifampin, pyrazinamide) is supplanted.
Time-Old triple Therapy:
The prolonged treatment of tuberculosis with streptomycin, isoniazid (INH) and paraaminosalicylic acid (PAS) extending for two years or more was widely and successfully used.
Present Recommended Therapy:
The above mentioned regimen is nowadays replaced by less toxic but equally effective drugs (in combination) with short course of therapy. The combined therapy consists of INH, rifampicin, pyrazinamide and ethambutol.
These are given orally and the duration of treatment is for 6 months. Pyrazinamide and ethambutol is stopped after 8 weeks. The treatment is continued for 8 months in non-respiratory tuberculosis. Direct observed treatment short course (DOTs) is conducted in India.
Alternative or second line anti-tuberculosis drugs widely used in developed countries are streptomycin, PAS, cycloserine and capreomycin. These drugs are both effective and cheap. When there is no improvement with therapy, sensitivity test for the infecting strain to a range of anti-tuberculous drugs is to be carried out.
6. Immuno-Prophylaxis (by BCG Vaccine):
Albert Calmette and Camittee Guerin (1921) prepared an attenuated strain of M. bovis by growing it on potato medium. The same strain was rendered completely avirulent by repeated subcultures, every 3 weeks for 231 times in glycerine potato medium in the course of 13 years.
When this strain found to be incapable to cause tuberculosis in susceptible guinea pigs, it was named as Bacille Calmette Guerin. (BCG) All BCG strains now used all over the world are derived from the original Bacille Calmette Guerin strain maintained at Pasteur Institute, Paris (France).
Any strain to be used for vaccine preparation has to be documented and approved by World Health Organisation (WHO). Pasteur 1173 P2, Tokyo—172, Copenhagen 1331 and Glaxo—1077 are four widely used strains.
The characteristics of the present strains of the BCG vaccine are:
(i) BCG strains grow well on glycerol containing medium
ADVERTISEMENTS:
(ii) They are aerobic
(iii) They are resistant to cycloserine.
7. Dose and Administration of BCG Vaccine:
BCG vaccine is available in:
(1) Liquid form, and
(2) Freeze-dried (lyophilized) form.
The freeze-dried vaccine supplied by BCG vaccine Laboratory, Chennai, is reconstituted by sterile physiological saline to make a final concentration of 0.1 mg (moist weight) in 0.1 ml of the vaccine; once reconstituted the vaccine should be readily used. The vaccine has become almost mandatory in developing countries.
a. Administration of the Vaccine:
The vaccine is given intradermally in a dose of 0.1 ml reconstituted BCG vaccine.
b. Age at Vaccination:
BCG vaccine should be administrated soon after birth, failing which it should be given at any time during the first year of life. WHO recommended routine use of BCG vaccine to all children below 15 years of age.
c. Observation of the Reaction:
At the site of vaccination a papule develops 2-3 weeks after intradermal injection of BCG, increases slowly in size and by about five weeks attains a diameter of 4 to 8 mm. Then the papule subsides and breaks into a shallow ulcer which heals up spontaneously leaving a 4 to 8 mm diameter permanent round ulcer.
Such individual becomes tuberculin positive after 4 to 6 weeks. The cell-mediated immune response lasts for 7-10 years. Prophylactic chemotherapy involves use of Isoniazid (INH) alone assuming that the bacillary load is very small and no chance of emergence of a drug-resistant mutant.