ADVERTISEMENTS:
The following points highlight the three processes of formation of urine in human body. The processes are: 1. Glomerular Filtration 2. Tubular Reabsorption 3. Tubular Secretion.
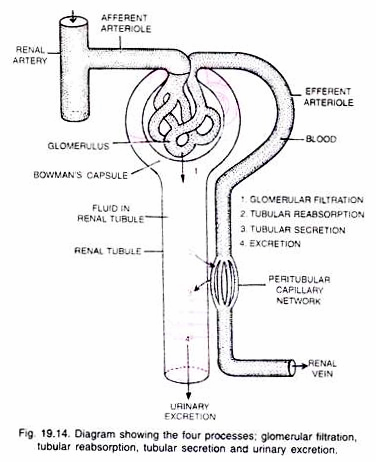
Process # 1. Glomerular Filtration (= ultrafiltration, Fig. 19.14):
On an average 1100-1200 ml of blood is filtered by the kidneys per minute. The glomerular capillaries are narrower than the afferent renal arterioles. Therefore, the blood pressure in the glomerular capillaries becomes very high so that there is continuous process of ultrafiltration (filtration under pressure) through the semi-permeable glomerular capillaries.
Thus water and many dissolved substances from the blood are filtered into the lumen of the Bowman’s capsule through its walls. The glomerular filtrate contains a large amount of water and other dissolved substances such as urea, uric acid, creatinine, amino-acids, glucose, sodium, potassium, vitamins, etc.
ADVERTISEMENTS:
The blood flows into efferent renal arterioles. Thus the glomerular filtrate and blood plasma are similar except that glomerular filtrate does not have proteins and fats.
The amount of the filtrate formed by both the kidneys per minute is called the glomerular filtration rate (GFR). In the normal person, the glomerular filtration rate is about 125 ml. per minute, i.e., 180 litres per day. Auto regulation of Glomerular Filtration. Three important intrinsic mechanisms provide auto regulation of glomerular filtration rate.
(i) Myogenic Mechanism:
ADVERTISEMENTS:
An increase in blood pressure, tends to stretch the afferent arteriole which increases the blood flow to the glomerulus. When the wall of the arteriole contracts, the diameter of the afferent arteriole is reduced that increases the flow of blood.
(ii) Juxtaglomerular Mechanism:
Juxtaglomerular apparatus (JGA) cells secrete enzymes like renin that modulate blood pressure and thus renal blood flow. This regulates GFR.
(iii) Neural Control:
Blood vessels of the kidney are innervated by nerve fibres of the sympathetic neural system. When activated, the nerve fibres bring about constriction of renal arteries and cause decrease in renal flow and glomerular filtration rate.
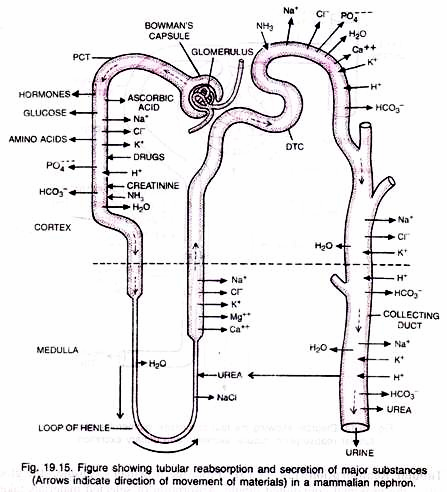
Process # 2. Tubular Reabsorption (Fig. 19.15):
From the Bowman’s capsule, the glomerular filtrate enters the proximal convoluted tubule. Absorption of selected materials takes place from the filtrate into the blood of the peritubular capillaries or vasa recta. It is termed the tubular reabsorption.
Reabsorption involves both passive and active transport across the tubular epithelium. As already stated, the glomerular filtrate in the Bowman s capsule resembles blood plasma in composition except for plasma proteins and fats. Therefore, it is almost isotonic to the plasma.
(i) Proximal Convoluted Tubule (PCT):
ADVERTISEMENTS:
About 65 per cent of the glomerular filtrate is normally reabsorbed in the proximal convoluted tubule before reaching the loop of Henle. Glucose, amino acids, vitamins, hormones, sodium, potassium, chlorides, phosphates, bicarbonates, much of water and some urea from the filtrate are absorbed.
Sulphates and creatinine are not reabsorbed. Sodium and potassium are reabsorbed by primary active transport. Glucose and amino acids are reabsorbed by secondary active transport. Water is reabsorbed by osmosis. Chloride ions, urea and other solutes are reabsorbed by diffusion. The filtrate is isotonic to blood plasma.
(ii) Loop of Henle:
ADVERTISEMENTS:
It consists of descending limb and ascending limb.
(a) Descending limb of loop of Henle:
As the filtrate flows in it, its water is reabsorbed due to increasing osmolality of interstitial fluid. Sodium and other solutes are not reabsorbed here. The filtrate becomes hypertonic to blood plasma.
(b) Ascending limb of loop of Henle:
ADVERTISEMENTS:
ADVERTISEMENTS:
It is impermeable to water but permeable to K+, Cl– and Na+ and partially permeable to urea. Thus in the thick ascending limb of the loop of Henle sodium, potassium, calcium, magnesium, and chloride are reabsorbed. The filtrate becomes hypotonic to blood plasma.
(iii) Distal convoluted tubules (DCT):
There is active reabsorption of sodium ions from the filtrate under the influence of aldosterone (hormone secreted by the cortex of adrenal glands). Chloride ions are also reabsorbed in the distal convoluted tubules. Water is reabsorbed here under the influence of antidiuretic hormone (ADH) secreted by posterior lobe of pituitary gland. This makes the filtrate isotonic to blood plasma.
ADVERTISEMENTS:
Collecting duct:
From distal convoluted tubule filtrate enters the collecting duct where further reabsorption of water takes place. Now the filtrate becomes more concentrated which makes filtrate hypertonic to blood plasma. The entire duct is permeable to water.
Thus a considerable amount of water is reabsorbed in the collecting duct under the influence of ADH. Sodium is reabsorbed in the collecting duct under the influence of aldosterone. The filtrate is now called urine. Thus urine is hypertonic to blood and isotonic to medullary fluid.
Some substances such as glucose and amino acids are reabsorbed actively into the blood by the active transport and, therefore, they do not appear in the urine. These substances are called the high threshold substances.
Renal threshold of a substance is its highest concentration in the blood up to which it is totally reabsorbed from the glomerular filtrate. The renal threshold of glucose is about 180 mg per 100 ml blood. When this value is exceeded, glucose begins to appear in the urine.
Process # 3. Tubular Secretion:
The cells of the renal tubule no. only remove substances from the filtrate by the process of reabsorption and send them to the blood capillaries (peritubular) but also excrete additional wastes from the blood stream into the filtrate by the process of secretion. Thus tubular secretion is the opposite of tubular reabsorption.
ADVERTISEMENTS:
It occurs as follows:
(i) Creatinine, hippuric acid, pigments, drugs including penicillin are actively secreted into the filtrate in the proximal convoluted tubule from the interstitial fluid. Hydrogen ions and ammonia are also secreted into the proximal convoluted tubule.
(ii) Urea enters the filtrate by diffusion in the thin segment of the ascending limb of loop of Henle.
(iii) Potassium, hydrogen ions, ammonia, HCO3” ions are secreted by active transport into the filtrate in the distal convoluted tubule.
Maximum hydrogen secretion occurs in the proximal convoluted tubule. Removal of hydrogen ions and ammonia from the blood in the proximal convoluted tubule and distal convoluted tubule helps to maintain the pH of the blood between 6 to 8 (pW of blood is usually 7.4)
Tubular secretion probably plays a minor role in the function of human kidneys but in animals like marine fishes and desert amphibians, whose nephrons do not possess developed glomeruli, their urine is formed mainly by the tubular secretion of urea, creatinine and mineral ions. Kidneys excrete about 1.5 litres of urine in a day.