ADVERTISEMENTS:
Read this essay to learn about: 1. Viral Infection that Cause Cancer 2. Bacterial Infections that Cause Cancer 3. Parasitic Infections that Cause Cancer.
Essay # 1. Viral Infections that Cause Cancer:
Discovery of Cancer Virus in Animals:
The idea that viruses can cause cancer was first proposed in the early 1900s. Although the role of chemicals and radiation in causing cancer was already recognized at the time, the possibility that infectious agents might also be involved was not seriously considered because cancer did not seem to behave like a contagious disease.
ADVERTISEMENTS:
However, in 1908 Danish scientists Wilhelm Ellerman and Olaf Bang reported that leukemia could be transmitted to healthy chickens by injecting them with blood extracts obtained from chickens that already had the disease.
Shortly thereafter Peyton Rous discovered that sarcomas could likewise be transmitted between chickens by injection of filtered tumor extracts. The latter experiments, led Rous to conclude that chicken sarcomas are transmitted by an infectious pathogen, and he eventually isolated several cancer viruses from chickens brought to him by local farmers.
Despite the clarity of Rous’s data, his work was initially greeted with skepticism and many years passed before the existence of oncogenic viruses (cancer- causing viruses) came to be widely accepted. Convincing proof required researchers to demonstrate the existence of other viruses that can cause cancer.
One of the first successes was reported in 1933, when Richard Shope showed that he could transmit skin cancer between rabbits using tumor extracts containing no intact cells. Such extracts contained an oncogenic virus subsequently named the Shope papillomavirus.
ADVERTISEMENTS:
In the following year, Baldwin Luck observed that kidney tumors in New England frogs could be transmitted in a similar fashion. And a few years later, John Bittner reported that breast cancer in mice is transmitted from mother to offspring by a virus present in breast milk.
In the following decades, dozens of additional oncogenic DNA and RNA viruses were discovered (Table 1). Most are selective in the hosts they infect and in the types of tumors they cause, although there are exceptions to this rule.
The murine polyomavirus, for example, infects a variety of mammals and causes more than 20 kinds of tumors, including cancers of the liver, kidney, lung, skin, bone, blood vessels, nervous tissues, and connective tissues.
A common feature shared by many oncogenic viruses is the ability to conceal themselves inside cells in a hidden or latent form in which no new virus particles are produced or released. Some latent viruses do not become active until the cell in which they reside is exposed to an appropriate stimulus, such as radiation, toxic chemicals, hormones, or even other viruses.
An example is provided by the feline leukemia virus, which can be harbored by otherwise healthy cats for many years. Only upon exposure to a physically stressful situation, such as a respiratory infection, does the latent virus become activated and cause cancer. At the same time, large numbers of new virus particles are produced and released, thereby triggering a potential cancer epidemic among neighboring cats.
The Epstein – Barr Virus:
By the late 1950s many viruses had been shown to cause cancer in animals, but no human examples were yet known. The situation was about to be changed, however, by the astute observations of a British surgeon named Denis Burkitt, who was running a medical clinic in Africa. Periodically, large numbers of children came to Burkitt’s clinic with massive swellings of the jaw, which he diagnosed as a lymphocytic cancer now called Burkitt’s lymphoma.
When Burkitt mapped the geographical distribution of the disease, he discovered that it only appeared in a region of Africa stretching between 10 degrees north of the equator and 10 degrees south, with a tail down the east coast (Figure 1). Because the rainfall and temperature patterns in this area make mosquito-transmitted infections exceptionally frequent, Burkitt proposed that the lymphoma was being transmitted by a mosquito-borne infectious pathogen.
Burkitt’s ideas soon attracted the attention of two virologists, Michael Anthony Epstein and Yvonne Barr, whose electron microscopic studies revealed virus particles in tumor cells isolated from patients with Burkitt’s lymphoma (Figure 2). The virus, identified as a member of the DNA-containing herpes virus group, is now called the Epstein-Barr virus (EBV) in recognition of the scientists who discovered it.
Unlike the situation with animal viruses, it is difficult to prove that a virus such as EBV causes cancer because ethical constraints prevent direct testing of the hypothesis by injecting the virus into healthy individuals. Nonetheless, several lines of evidence support the idea that EBV causes Burkitt’s lymphoma.
First, DNA sequences and proteins encoded by EBV have been found in tumor cells obtained from patients with Burkitt’s lymphoma but not in normal cells from the same individuals.
ADVERTISEMENTS:
Second, adding EBV to cultures of normal human lymphocytes stimulates cell proliferation and causes the lymphocytes to acquire some of the traits of cancer cells.
Finally, injecting EBY into monkeys triggers the development of lymphomas.
Although the evidence linking EBV to Burkitt’s lymphoma is strong, the story is not quite so simple. We now know that EBV is a ubiquitous virus that has infected more than 90% of the world’s population.
If the virus is so common, why is Burkitt’s lymphoma concentrated in a few geographical locations, such as central Africa, and infrequent elsewhere? A possible answer is suggested by research showing that Burkitt’s lymphoma only appears in regions of Africa where the disease malaria is prevalent and childhood immunity has been depressed by malarial infection.
ADVERTISEMENTS:
The role of mosquitoes in Burkitt’s lymphoma is thus indirect; by spreading malaria, mosquitoes cause a disease that depresses immune function and thereby allows EBV infections to proceed unchecked by an effective immune response.
The idea that a deficient immune response plays a permissive role in allowing EBV-induced lymphomas to arise has received independent support from studies involving AIDS patients, whose immune systems are also debilitated. As we will see shortly, individuals with AIDS have abnormally high rates of several kinds of cancer, including lymphomas.
Burkitt’s lymphoma is not the only kind of lymphocytic cancer to be linked to EBV infection. Based on differences in their appearance, lymphomas are commonly subdivided into a dozen or more subtypes.
One prominent form, called Hodgkin’s disease, is a lymphoma characterized by the presence of Reed-Sternberg cells, which possess two nuclei and have a uniquely distinctive appearance. A role for EBV in Hodgkin’s disease is suggested by the finding that about half the patients with this cancer have EBV DNA sequences in their tumor cells.
ADVERTISEMENTS:
In addition to its involvement in lymphocytic cancers, EBV infection can also trigger a nonmalignant proliferation of lymphocytes known as infectious mononucleosis (or simply “mono”). Infectious mononucleosis produces temporary flu-like symptoms and occurs mainly in individuals whose first encounter with EBV takes place when they are teenagers.
If a person’s initial exposure to EBV happens earlier in life, it rarely produces disease symptoms. Because EBV is transmitted mainly through exchange of saliva, mononucleosis has been nicknamed the “kissing disease.”
Roughly half the individuals who are first exposed to EBV as teenagers develop the symptoms of mononucleosis, which include swollen lymph glands, fever, headache, muscle aches, and fatigue. While the condition is almost always self- limiting, individuals who have had mononucleosis exhibit a slightly elevated risk for developing Hodgkin’s disease or other lymphomas.
EBV Infection:
Lymphocytes are not the only cells targeted for attack by EBV; the virus can also infect and trigger abnormal proliferation of epithelial cells. The clearest example of an epithelial cancer induced by EBV is nasopharyngeal carcinoma, a tumor of the nasal passages and throat that is frequent in Southeast Asia but rare elsewhere in the world.
In patients with nasopharyngeal carcinoma, EBV DNA is detected in their tumor cells but not in the cells of the surrounding normal epithelium, suggesting that the cancer arises from EBV-infected cells. While it is unclear why nasopharyngeal carcinoma is common in Southeast Asia but not elsewhere, hereditary or dietary factors unique to that part of the world may play a role in determining susceptibility.
ADVERTISEMENTS:
Even though 90% of the world’s population has been exposed to EBV, cells infected by the virus rarely become malignant and little evidence implicates EBV in most of the common epithelial cancers. A small percentage of individuals with stomach or breast cancer do have EBV DNA sequences in their cancer cells, but the precise role played by EBV in such cases is not clear. Some evidence suggests that the presence of EBV may influence the behavior of cancer cells even when it is not the underlying cause of the disease.
For example, one protein produced by EBV binds to and inhibits the activity of a normal cellular protein called Nm23-H1. The Nm23-H1 protein, which inhibits cell migration, is produced by one of the cell’s metastasis suppressor genes. The ability of EBV to bind to and inhibit Nm23-H1 may enhance cancer cell motility and thereby facilitate the ability of cancer cells to invade and metastasize.
Human Papillomavirus as a Cause of Cervical Cancer:
EBV was the first oncogenic virus to be identified in humans, but it is not the virus that causes the most human cancers. That distinction belongs to human papillomavirus (HPV), a DNA virus implicated in cancer of the uterine cervix (cervical cancer) and in several other cancers of the anal and genital area, including cancer of the penis.
The idea that cervical cancer is triggered by an infectious agent can be traced back to the nineteenth century, when epidemiologists first noted that cervical cancer is relatively common in prostitutes but unknown in nuns.
Such observations led to the suggestion that cervical cancer is a sexually transmitted disease, an idea now supported by much additional evidence. For example, cervical cancer rates are elevated in women who have had multiple sexual partners and in women who have sexual relationships with men who were previously married to women who developed cervical cancer.
ADVERTISEMENTS:
Although the idea that cervical cancer is caused by a sexually transmitted pathogen was first proposed more than one hundred years ago, not until the 1980s did evidence begin to point to HPV as the responsible agent. The situation was initially complicated by the fact that HPV is not a single virus but a heterogeneous family of related viruses consisting of more than 100 different types (designated HPV 1, HPV 2, HPV 3, and so forth).
As methods for identifying the various types of HPV improved, some striking patterns began to emerge. Epidemiological studies revealed that certain forms of HPV, designated high-risk types, are consistently associated with cervical cancer.
The most prevalent member of this group, HPV 16, is detected in roughly half of all cervical cancers, followed in frequency by HPV 18, HPV 45, HPV 31, and a small group of others (Figure 3). In worldwide studies of cervical cancer, about 90% of the cases have been found to involve at least one of these high-risk types of HPV.
Other forms of HPV are considered to be low-risk types because they are associated with nonmalignant conditions; for example, HPV 6 and HPV 11 are a common cause of tiny skin-colored bumps, called genital warts, in the male or female genital area.
Roughly 50% of all women become infected with HPV sometime during their life. Most infections are transient and disappear within a year or two, but a small fraction of the infections involving high-risk forms of HPV become persistent. Over a period of many years, persistent infections can trigger cervical dysplasia that, if untreated, eventually develops into cancer.
Of the various risk factors that influence the likelihood that an infection will persist and progress to cervical cancer, cigarette smoking is the strongest. Epidemiological studies of HPV-infected women have revealed that cigarette smokers are up to four times more likely to develop cervical cancer than are women who have never smoked.
The evidence also suggests that normal immune function can help protect against the development of cervical cancer; in organ transplant patients treated with immunosuppressive drugs to decrease the risk of immune rejection of the transplanted organ, cervical cancer rates are ten times higher than normal.
The Hepatitis B and Hepatitis C Viruses as a Cause of Liver Cancer:
The disease known as hepatitis—inflammation of the liver—was first recognized thousands of years ago based on the distinctive yellow color imparted to a person’s skin when the liver fails to metabolize and excrete pigments properly.
In recent years, diagnosis of hepatitis has become more refined and doctors can now distinguish between several forms of the disease; some are triggered by the toxic effects of alcohol or drug consumption, whereas others are caused by viruses. At least six hepatitis viruses are known to exist, two of which are strongly linked to the development of liver cancer.
The largest number of cancers stem from infection with hepatitis B virus (HBV), a DNA virus first detected in hepatitis patients around 1970. HBV is usually transmitted by exchange of bodily fluids, such as semen or blood. The virus has infected more than 300 million people worldwide and is responsible for more than 75% of the world’s cases of liver cancer.
People infected with HBV are about 100 times more likely to develop liver cancer than are those who have never been infected. Infections are especially prevalent in Southeast Asia, China, Africa, Alaska, northern Canada, and the Amazon River basin of South America (Figure 4). In these regions of the world, close to 10% of the population is infected with HBV, and liver cancer is one of the most frequently encountered cancers.
HBV-induced liver cancers only arise after individuals have been infected for many years. A key factor in determining whether a person will develop such a persistent infection is the age when initially infected.
Roughly 90% of all children infected at birth become chronically infected, but the value falls to 25% for infections occurring up to the age of 5 years and continues to decline as infections occur later in life. This gradual improvement in a person’s resistance to chronic infection may result from changes in the ability of the immune system to restrain the virus, but the exact mechanism is not clear.
The other virus linked to liver cancer is hepatitis C virus (HCV), an RNA-containing virus discovered in 1988. In contrast to HBV, which is easily spread through sexual activity, HCV is difficult to transmit by mechanisms other than direct contact with contaminated blood. Because blood used for medical transfusions is routinely screened for HCV (and HBV) contamination, the main route for acquiring HCV is through the sharing of dirty needles by intravenous drug users.
Blood-screening techniques for identifying HCV were not introduced until 1990, however, which means that millions of people who received blood transfusions prior to that time were at risk of being infected with HCV As a consequence, HCV is being carried by several million people in the United States, most of whom do not realize that they are infected.
Although HCV is more difficult to transmit than HBV, a larger number of people in the United States are infected with HCV (about 1.8% of the population) than with HBV (about 0.5% of the population). The explanation for this apparent contradiction is that HCV has a greater tendency to trigger long-term, chronic infections than does HBV.
Less than 25% of the individuals infected with HBV develop chronic infections, whereas 75% of those infected with HCV will do so. More people therefore end up being chronic carriers of HCV. Roughly 5% of the people with chronic HCV infections eventually develop liver cancer, although it usually requires several decades to appear.
The HTLV-I Retrovirus as a Cause of Adult T-Cell Leukemia and Lymphoma:
In animals, many of the viruses that cause cancer are members of the retrovirus family. Retroviruses contain RNA as their genetic material packaged along with reverse transcriptase, an enzyme that synthesizes a DNA copy from the RNA’s base sequence. Making a DNA copy allows the viral genes to become integrated into the chromosomal DNA of an infected host cell.
Dozens of retroviruses have been shown to cause cancer in animals, but only one has been clearly linked to human cancer. This virus, called human T-cell lymphotropic virus-I (HTLV-I), was first identified in 1980 in lymphocytes obtained from patients with adult T-cell leukemia/lymphoma, a particularly aggressive type of cancer that is rare in the United States but prevalent in certain parts of Japan, Africa, and the Caribbean.
Infection with HTLV-I is so tightly linked to adult T-cell leukemia/lymphoma that the presence of the virus is one of the diagnostic criteria for identifying this particular kind of cancer, HTLY-I is transmitted mainly through sexual contact, through blood products, and from mother to child during breast-feeding.
In regions of the world where HTLV-I is prevalent, up to 10% of the population may be infected. Cancer develops in only a few percent of infected individuals; it usually arises many decades after initial infection and is more common among those infected early in life.
Increased Risk for Kaposi’s Sarcoma and Several Other Viral Cancers in HIV-Infected Individuals:
HTLV-I is the only retrovirus to be directly implicated in causing a human cancer, but the well-known retrovirus HIV (human immunodeficiency virus) represents an indirect cancer risk because of its destructive effects on the immune system. HIV-infected individuals who develop the symptoms of acquired immunodeficiency syndrome (AIDS) have a debilitated immune system that puts them at increased risk for several types of cancer (Figure 5).
The greatest risk is for Kaposi’s sarcoma, a cancer arising from blood vessels in the skin. Kaposi’s sarcoma is generally quite rare in the United States, but rates are increased 100-fold in people infected with HIV. Reports of a sudden increase in these unusual, reddish purple skin tumors in Los Angeles and New York City in 1981 were one of the earliest signs heralding the onset of the AIDS epidemic.
By 2004 it was estimated that 40 million people worldwide were infected with HIV, and in some regions of Africa, where more than 20% of the adult population is infected, Kaposi’s sarcoma has become the most common type of cancer.
In 1994, a DNA virus called Kaposi’s sarcoma- associated herpesvirus or KSHV (also known as human herpesvirus-8 or HHV-8) was discovered in specimens of Kaposi’s sarcoma tissue. KSHV is a sexually transmitted virus that exhibits a number of properties suggesting a causative role in Kaposi’s sarcoma.
For example, KSHV is found in virtually all Kaposi’s sarcoma tumors, it specifically targets the cell type that becomes cancerous, and infection with KSHV precedes tumor development. KSHV infection by itself, however, is not sufficient to cause cancer; some degree of immune deficiency, as occurs in AIDS, is also required.
Evidence for the role of immune deficiency in permitting Kaposi’s sarcoma to develop has come from studies of AIDS patients treated with drug cocktails known as highly active antiretroviral therapy (HAART). In those individuals whose immune function improves in response to HAART treatment, Kaposi’s sarcoma often disappears.
While the increase in cancer risk is most dramatic for Kaposi’s sarcoma, this is only one of several viral cancers to occur at higher-than-normal rates in people with HIV/AIDS. Lymphomas triggered by infection with EBV or KSHV, cervical and skin cancers induced by HPV, and liver cancer triggered by HBV or HCV are other viral Canters whose incidence increases in individuals whose immune systems have been debilitated by HIV.
SV40:
Between 1955 and 1963, batches of polio vaccine that were used to immunize hundreds of millions of people around the world, including almost 100 million people in the United States, were unknowingly contaminated with a monkey virus called SV40 (an abbreviation for simian virus 40).
SV40 was present in the monkey kidney cells that had been used to grow the polio virus, but scientists did not know it was there and so had not taken steps to remove it. When the polio vaccine was manufactured, the procedures that were designed to inactivate the polio virus did not fully inactivate the SV40 that contaminated the vaccine.
SV40 was removed from the vaccine as soon as the virus was discovered, but concerns have persisted about the possible health consequences for the millions of people who were inadvertently exposed to the monkey virus.
Animal and laboratory testing has not been reassuring: SV40 triggers the development of several types of cancer in animals and causes cultured human cells to develop some of the traits of cancer cells. Such findings raise the alarming possibility that the vaccine that eradicated polio in the United States might have inadvertently caused an outbreak of cancer.
Fortunately, four decades of epidemiological studies have failed to reveal any significant increases in cancer rates among people exposed to the contaminated polio vaccine. It is still possible, of course, that SV40 caused smaller numbers of cancers that cannot be reliably detected using epidemiological approaches.
Investigators using an alternative tactic have discovered that SV40 DNA sequences are sometimes detectable in the cancer cells of individuals with non-Hodgkin’s lymphoma, mesothelioma, brain cancer, or bone cancer. Although such data do not prove that the virus actually caused these tumors, it is interesting to note that the same four kinds of cancer are triggered by SV40 in animals.
Additional concerns are raised by the discovery that many people with SV40 DNA in their tumor cells were never vaccinated with the contaminated polio vaccine, suggesting that SV40 might be spreading from person to person. The methods used for detecting tiny amounts of SV40 in cancer cells are fraught with difficulties, however, and the reliability of the data is open to question.
For the moment, we do not really know how much (if any) cancer risk was created by the inadvertent exposure of humans to SV40. Nevertheless, the failure of the epidemiological data to demonstrate a relationship between exposure to the contaminated vaccine and cancer risk suggests that any hazards that might have been created are relatively small.
Essay # 2. Bacterial Infections that Cause Cancer:
Infection with the Bacterium Helicobacter Pylori is Linked to Stomach Cancer:
In contrast to viruses, whose roles in causing cancer have been studied for almost one hundred years, the possible cancer risks associated with chronic bacterial infections were not recognized until quite recently. One bacterium that has now been clearly linked to a human cancer is Helicobacter pylori, also known as H. pylori.
This spiral-shaped bacterium was initially isolated in 1982 from the stomachs of people suffering from gastritis, an inflammation of the stomach lining that represents the first step in the development of stomach ulcers.
To determine whether H. pylori are the underlying cause of gastritis, one of the investigators who discovered the organism, Barry Marshall, deliberately swallowed a sample of H. pylori himself. Marshall had been healthy prior to ingesting the bacteria, but he soon developed gastritis.
During the following decade, epidemiological studies began to reveal a strong connection between stomach cancer and exposure to H. pylori. It was found that H. pylori infections are present prior to the appearance of stomach cancer and that stomach cancer only develops in people who have had such an infection.
Laboratory studies eventually confirmed the relationship by showing that mice deliberately infected with H. pylori develop stomach cancer. Although the way in which H. pylori contributes to cancer development is not completely understood, the bacterium is known to secrete toxins and cause inflammation in the stomach, which in turn stimulates cell proliferation and triggers DNA damage.
Over a period of many years the proliferating cells become progressively more abnormal, creating areas of dysplasia that eventually develop into cancer. Because it is linked to a bacterial infection, stomach cancer can usually be prevented by treating infected individuals with antibiotics to rid them of H. pylori. Antibiotics even reduce the rate of cancer recurrence in stomach cancer patients who are treated after their tumors have been removed.
H. pylori has infected at least half the world’s population, making stomach cancer one of the most common cancer killers worldwide, second only to lung cancer. Nevertheless, significant global variations exist in the prevalence of both H. pylori and stomach cancer. In the United States, stomach cancer rates have been declining for many decades, making the disease less common than in most other countries.
One factor contributing to these low stomach cancer rates is the widespread use of antibiotics, which decreases the prevalence of H. pylori infections. Public health conditions also play an important role because transmission of H. pylori from person to person is facilitated by poor sanitation and crowded living environments, which are more frequently encountered in developing countries than in the United States.
As a result, H. pylori infections are less frequent in the United States than in many other parts of the world, and infections tend to occur later in life, when they are associated with a lower risk of causing stomach cancer (Figure 6).
Of the millions of people infected with H. pylori worldwide, only a few percent develop stomach cancer. It is not clear why such a small percentage of H. pylori infections lead to cancer, but several factors are thought to play a role. One variable is the type of bacterial strain involved. H. pylori are heterogeneous group of bacteria, and a single infected person often carries multiple bacterial strains that change with time.
The risk of developing cancer may depend to a significant extent on the type of H. pylori that prevails. Differing immune responses to the various bacterial strains can influence the course of infection, and blood type also plays a role because H. pylori adheres to the stomach lining by binding to cell surface receptors that are related to a person’s blood type.
Some strains of H. pylori adhere preferentially to receptors associated with blood type O, making individuals with this blood type more susceptible to chronic H. pylori infections than individuals with other blood types.
Diet is another factor that influences the likelihood that exposure to H. pylori will lead to chronic infection and cancer. Stomach cancer rates are highest in those regions of the world, such as Japan, China, and Latin America, where diets are very salty because meat, fish, and vegetables preserved by salting are traditionally eaten on a regular basis. In animal studies, high-salt diets have been shown to enhance the ability of H. pylori to infect the stomach lining and stimulate cell proliferation.
Essay # 3. Parasitic Infections that Cause Cancer:
Flatworm Infections Leads to Cancers of the Bladder and Bile Ducts:
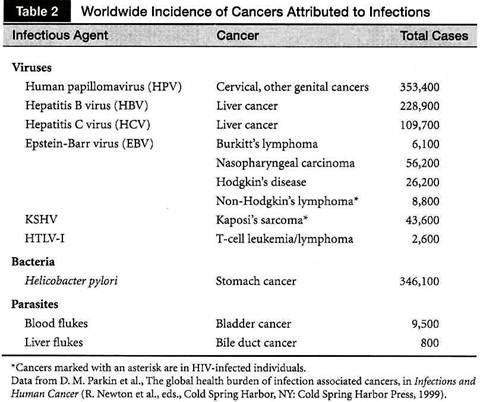
The final group of infections that pose a cancer hazard involve parasitic flatworms. Compared with viral and bacterial infections, which are linked to more than a million cases of cancer worldwide each year (Table 2), the cancer burden associated with parasitic infections is quite small, although it still involves about 10,000 cases of cancer annually.
The biggest risk is posed by blood flukes, which are tiny flatworms that cause the disease schistosomiasis in tropical and subtropical regions of the world, mainly in Africa. Blood flukes are carried by freshwater snails, which harbor the larvae of the parasite.
When people bathe in water contaminated by infected snails, the larvae penetrate the skin and, after maturing, settle in the blood vessels of the intestine or bladder, where they cause chronic inflammation. Most of the fatalities associated with schistosomiasis come from kidney or liver failure, but chronic inflammation of the bladder occasionally leads to bladder cancer.
Another type of parasitic flatworm, called a liver fluke, resides mainly in Asia and is acquired by eating raw or undercooked fish. The ingested parasite moves from the intestines into the bile ducts, where it becomes lodged in the smaller ducts of the liver and triggers local inflammation. Such infections can eventually lead to the development of bile duct cancer (cholangiocarcinoma), which is very rare in most parts of the world but occurs more frequently in regions of Asia where liver fluke infections are common.